Effects of pregnancy intention, interpregnancy interval and postpartum contraception uptake on child survival: insights from the Indian demographic health surveys | BMC Pregnancy and Childbirth

Descriptive statistics
Table 1 summarizes descriptive frequencies showing the sample distribution of the selected socio-economic, demographic and program-related characteristics. The results clearly showed that over 90% of women were between the ages of 20–24 years at last birth during this period. More than half, 52.5% (2015–16) and 51.1% (2019–21) of the infants were male. With respect to various uptake of maternity services, young women who had attended ≥ 4 ANC visits increased by 5% (from 49.4 to 54.4%), followed by institutional birth increased by 7.7% (from 82.5 to 90.2%), C-sectional delivery rose by 2.3% (from 16.6 to 18.9%) and PNC check-up for mother within 42 days increased by 13.6% (from 69.1 to 82.7%), respectively. A significant proportion of respondents WHO faced difficulty accessing the nearest health facility for minor and big problems declined slightly by 5.3%, from 70.2% in 2015–16 to 64.9% in 2019–21. In both NFHS rounds, almost 91% of the children in each survey sample had breastfed. Notably, respondents WHO had received full exposure to media decreased by 13.4%, from 66.5% in 2015–16 to 53.2% in 2019–21. With respect to educational attainment, the proportion of women WHO had received no formal education decreased by 4.7% (from 21.9 to 17.2%), followed by primary education (3.8%, from 15 to 11.2%), whereas the proportion of women WHO had attended secondary education increased by 6.1% (from 55.6 to 61.7%), followed by higher education (2.5%, from 7.5 to 10%), respectively. Regarding social status, both OBC and SC/ST were the most dominant socially disadvantaged groups. In terms of household’s wealth status, nearly 72% in 2015–16 and 74% in 2019–21 of young women belonged to the lowest three wealth quintiles, while the richer and richest quintiles stayed almost stable over time. Respondents concerning their religion and child’s parity remained almost stable over time; nearly 83% belonged to the Hindu religion; over 40% had first, and 42% had second parity of children. Lastly, over three-fourth of respondents (76.7% in 2015–16 and 80.9% in 2019–21) lived in rural counterparts.
Prevalence of child survival, pregnancy intention, interpregnancy interval and postpartum contraception uptake
With respect to infant mortality, only 3.8–3.4% (declined by 0.4%) of infants died during the first year after birth between 2015 and 16 and 2019-21, respectively. However, Fig. 1 illustrates the proportion of pregnancy intention, IPI and postpartum contraception uptake among young married women in India. Approximately 92% of all young women reported that their pregnancies were wanted between 2015 and 16 and 2019-21. In terms of unintended pregnancy, only 6% and 6.5% (increased by 0.5%) of young women reported mistimed pregnancies, while only 2.0% and 1.7% (decreased by 0.3%) reported that their pregnancies were unwanted over time, respectively. Concerning the duration of various IPIs, women with IPI of at least 24 months had significantly increased by 4.2%, from 24.4% in 2015-16 to 28.6% in 2019-21. During this period, women with IPI of 7–24 months had slightly declined by only 2.3% (from 58.4 to 56.1%), while an IPI of 6 months or less had dropped by 1.9% (from 17.2 to 15.3%). Interestingly, Fig. 1 shows that the proportion of postpartum modern contraception adoption within first 12 months after a recent childbirth among young women had sharply climbed by 9%, from 33% in 2015-16 to 42% in 2019-21.
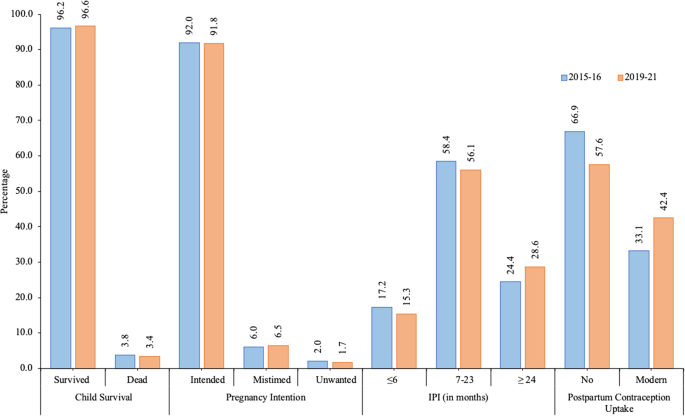
Percentage of child survival among infants and pregnancy intention, interpregnancy interval and postpartum modern contraception uptake among young married women, India, NFHS, 2015-16 and 2019-21
Results from survival analysis
The graphical illustrations in Figs. 2 and 3 highlighted insights into key features of the differences in K-M survival functions for child survival among infants by pregnancy intention, IPI and postpartum contraception uptake. It is worth mentioning that the K-M curves differed substantially for various categories of postpartum contraception uptake, followed by pregnancy intention and IPI between 2015 and 16 and 2019-21. For instance, the probability of infant survival was highest amongst young women who had adopted postpartum modern contraception compared to those who had not used any contraception over time (Figs. 2 and 3). Furthermore, a Log-rank test was applied to examine the significance of the observed differences in K-M survival curves for various categories of the selected variables.
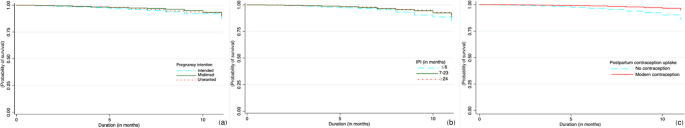
Kaplan-Meier survival curves for child survival among infants by pregnancy intention (a), interpregnancy interval (b) and postpartum contraception uptake (c), India, NFHS, 2015-16
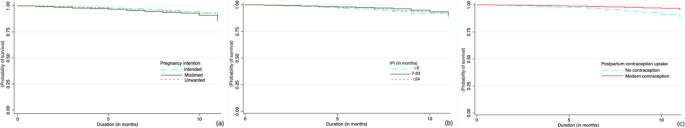
Kaplan-Meier survival curves for child survival among infants by pregnancy intention (a), interpregnancy interval (b) and postpartum contraception uptake (c), India, NFHS, 2019-21
The results of the Log-rank test for the key explanatory variables and selected background characteristics of respondents (mother’s age at last birth, child’s sex, parity, number of ANC visits, PoD, MoD, PNC check-up, breastfeeding, distance to nearest health facility, exposure to media, level of education, religion, caste, wealth quintile and place and region of residence) were shown in Table 2. Barring child’s sex, number of ANC visits, distance to nearest health facility, religion, caste and place of residence in NFHS-4, and mother’s age at last birth, MoD, distance to nearest health facility, religion, caste and place of residence in NFHS-5, significant differences in survival time among infants for various categories of selected demographic and socio-economic characteristics were observed. Although the Log Rank test determined if there were any significant variances between two groups, it did not assure how much difference they were actually. For this reason, the Cox-PH models were applied in the present analyses to address this gap.
Effects of pregnancy intention, interpregnancy interval and postpartum contraception uptake on infant mortality
The results of Cox-PH regression models showing the UHR and AHR of infant mortality by key explanatory variables and selected socio-economic, demographic and program-related factors were presented in Tables 3 and 4. The unadjusted results highlighted the contribution of each variable on infant mortality during the specified time period. Conversely, the adjusted results revealed key insights into the changes in the effects of pregnancy intention, IPI and postpartum contraception uptake on infant mortality while controlling for several potential correlates.
In Table 3, pregnancy intention, IPI and postpartum contraception uptake were significantly associated with infant mortality even after adjusting for socio-economic, demographic and program-related factors, hinting that the strength of associations remained same and strongly valuable in explaining the differentials in the likelihood of infant mortality in both bivariate and multivariate Cox regression models. Like unadjusted results, the adjusted results in Table 3 revealed that young women who had mistimed (AHR: 0.678, 95% CI: 0.421–1.092) and unwanted (AHR: 0.882, 95% CI: 0.498–1.564) pregnancies, IPI of 7–23 months (AHR: 0.901, 95% CI: 0.673, 1.207) and 24 months or more (AHR: 0.811, 95% CI: 0.566–1.162), and adopt postpartum modern contraception (AHR: 0.517, 95% CI: 0.335–0.798) were significantly associated with a reduced relative risk of infant mortality compared to those WHO had wanted pregnancy, IPI of less than or 6 months and no contraception uptake.
Furthermore, the results in bivariate Cox-PH models identified that mother’s aged 20–24 years at last birth, had second parity, 4 or more ANC visits, institutional birth, c-section delivery, PNC check-up within 42 days, had breastfed, full exposure to media, attended secondary and higher education, affiliated with Muslim religion, belonged to the middle, richer and richest quintiles and resided in the West and Sothern regions were significantly associated with a reduced relative risk of infant mortality. Interestingly, even after adjusting for socio-economic, demographic and program-related factors, a significantly lower likelihood of infant mortality was observed among mother’s aged 20–24 years at last birth (AHR: 0.478, 95% CI: 0.310–0.738), had institutional birth (AHR: 0.786, 95% CI: 0.546–1.131), PNC check-up within 42 days (AHR: 0.944, 95% CI: 0.681–1.308), had breastfed (AHR: 0.001, 95% CI: 0.002–0.004), affiliated with OBC (AHR: 0.768, 95% CI: 0.575–1.028), belonged to the middle (AHR: 0.778, 95% CI: 0.534–1.133), richer (AHR: 0.619, 95% CI: 0.378–1.013) and richest (AHR: 0.549, 95% CI: 0.243–1.241) quintiles and lived in the East (AHR: 0.846, 95% CI: 0.533–1.341), West (AHR: 0.834, 95% CI: 0.427–1.629) and Southern (AHR: 0.459, 95% CI: 0.240–0.879) regions compared to mother’s aged 15–19 years at last birth, had given birth at home, no PNC check-up, never breastfed, belonged to SC/ST and poorest quintile, and resided in the Northern region. Unlike bivariate Cox models, the multivariate results revealed that factors, namely, distance to nearest health facility, media exposure, religion and place of residence, did not show any significant effects on infant mortality.
In Table 4, the results demonstrated that pregnancy intention, IPI and postpartum contraception uptake emerged as the key significant factors associated with infant mortality even after controlling for a range of potential correlates. Like unadjusted results, the adjusted results (Table 4) further revealed that the relative risk of infant mortality was significantly lower among women who had unwanted pregnancy (AHR: 0.488, 95% CI: 0.208–1.146), IPI of 7–23 months (AHR: 0.886, 95% CI: 0.621–1.264) and 24 months or more (AHR: 0.917, 95% CI: 0.628, 1.338), and postpartum modern contraception uptake (AHR: 0.429, 95% CI: 0.276–0.667) compared with those WHO had mistimed pregnancy, IPI of less than or 6 months and no contraception uptake.
Like Table 3, the bivariate Cox results (Table 4) highlighted similar findings. After controlling for socio-economic, demographic and program-related factors, a significantly lower likelihood of infant mortality was observed among mothers WHO had PNC check-up within 42 days (AHR: 0.662, 95% CI: 0.426–1.029), had breastfed (AHR: 0.003, 95% CI: 0.005–0.009), attended higher education (AHR: 0.934, 95% CI: 0.412–2.117), belonged to the richest quintile (AHR: 0.267, 95% CI: 0.107–0.663), and lived in the Central (AHR: 0.934, 95% CI: 0.532, 1.640) and Southern (AHR: 0.396, 95% CI: 0.188, 0.836) regions compared to mothers with no PNC check-up, never breastfed, illiterate, belonged to poorest quintile and resided in the Northern region. Unlike bivariate results, the multivariate results found that child’s sex and caste were not associated with infant mortality.
However, Tables 3 and 4 show that pregnancy intention, IPI and postpartum contraception uptake were strongly associated with infant mortality even after controlling for many potential correlates. The results further highlighted several conflicting findings between 2015 and 16 and 2019-21. Surprisingly, no significant differences in infant mortality were observed with respect to child breastfeeding in both NFHS rounds. Unlike Table 4 (bivariate Cox models), the results in Table 3 showed that respondents who had delivered C-section birth, affiliated with Muslims and OBC, and resided in rural counterparts and the Eastern region were significantly associated with a reduced relative risk of infant mortality. Unlike Table 3, the multivariate results (Table 4) showed that mother’s aged 20–24 years at last birth, affiliated with OBC, belonged to the middle and richer quintiles and resided in the Eastern and Western regions were closely associated with a reduced relative risk of infant mortality.
link







