Factors related to postpartum length of stay in women with pre-eclampsia: a systematic review | BMC Pregnancy and Childbirth

Study selection
The initial search across selected databases yielded 2,580 studies. Among these, eight studies [10, 15,16,17,18, 20,21,22] met the inclusion criteria. Figure 1 provides an overview of the selection process, detailing the number of articles excluded at each stage of this systematic review.
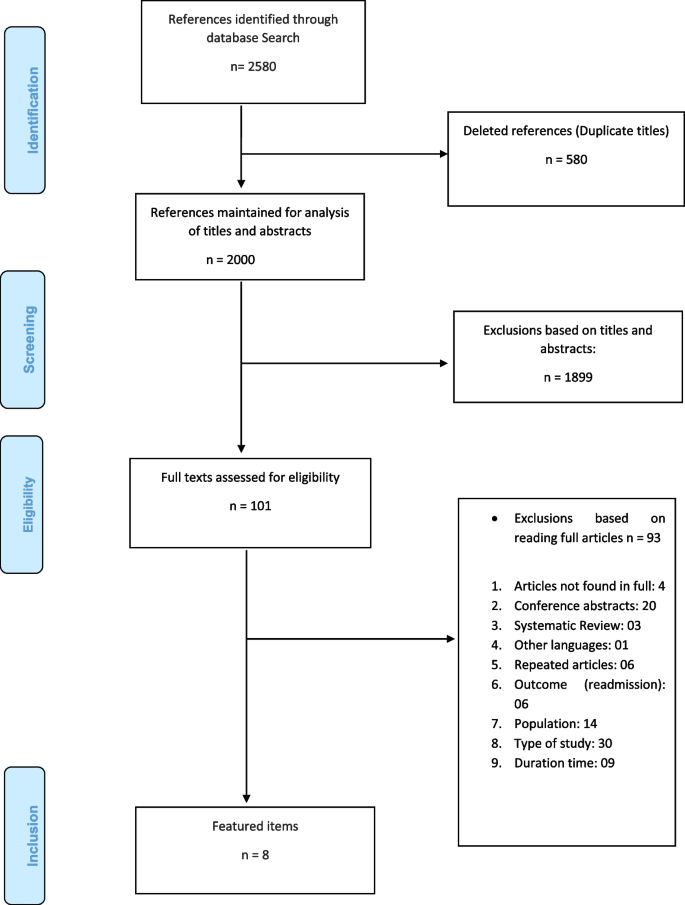
Flowchart of the study selection process
Characteristics of the studies
The selected studies spanned three continents: Asia (n = 3) [16, 18, 20], Africa (n = 1) [15], and America (n = 4) [10, 17, 21, 22]. These studies employed cohort [10, 15,16,17,18, 20,21,22] designs. The sample sizes ranged from 98 to 256,010 patients. All studies were conducted in local reference maternity hospitals, three of which were teaching maternity hospitals. Four studies focused on patients with severe preeclampsia [15, 17, 18, 20], while one study addressed eclampsia [16].
The patients in the selected studies had a mean age ranging from 23.4 to 35.5 years [10, 15,16,17,18, 20,21,22] and a minimum gestational age of 33.18 weeks, with the majority reaching full-term pregnancy at 37 weeks or more [10, 15,16,17,18, 20]. Two studies did not specify the gestation time [21, 22]. Further details of the study characteristics are detailed in Table 1.
This review identified multiple risk factors associated with prolonged postpartum hospitalization in women with preeclampsia, encompassing clinical, biochemical, and sociodemographic aspects. The findings are presented based on the type of risk factor, integrating evidence from studies with varying methodological designs and levels of confidence. Below, the key findings are organized by risk factor, providing a structured approach to the data interpretation. The factors identified in this review are represented in the following framework in Fig. 2.
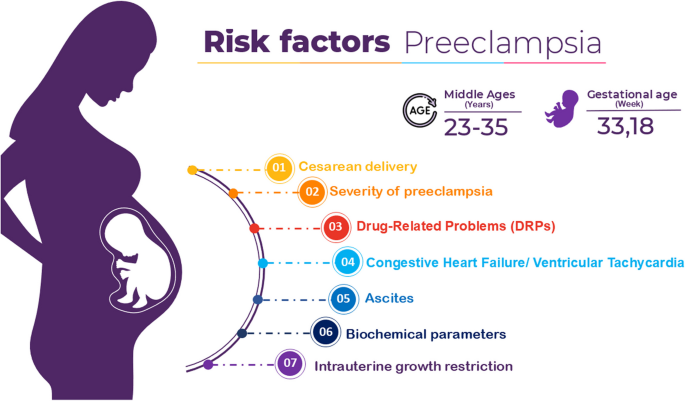
Framework the risk factors for length of stay in women with preeclampsia
Ascites
One significant risk factor for prolonged postpartum hospitalization was the presence of ascites, as reported in a cohort study by Mbonyizina et al. (2019), which included 112 patients diagnosed with severe preeclampsia. Ascites was identified in 60 patients (cases). Women with both antepartum and postpartum ascites experienced longer hospital stays (7.7 ± 0.52 vs. 5.4 ± 0.39 days, p < 0.001). Other factors, such as severe hypertension and altered biochemical parameters, were also identified, potentially contributing to the increased length of stay.
Cesarean delivery
Three studies 10,17,20 identified cesarean delivery as a potential risk factor for prolonged postpartum hospitalization. In the study by Amorin et al. (2014), the cesarean delivery rate was 68.2%, with an average hospitalization of 8 days for cesarean births compared to 5 days for vaginal births. Prolonged hospitalization was attributed to complications such as postpartum hemorrhage and increased blood pressure. Goes et al. (2021) also noted cesarean delivery as a factor increasing hospitalization, but this association was not statistically significant after adjusting for confounding factors. Li et al. (2022) reported an average hospitalization of 5.8 days for cesarean births, compared to 3.4 days for vaginal births. Prolonged hospitalization may result from complications and patient-related factors, such as comorbidities and the severity of preeclampsia. While these studies did not directly examine local practices, hospitals with limited resources may influence hospitalization duration.
Drug-Related Problems (DRPs)
Another risk factor identified in the study by Goes et al. (2021) was the presence of drug-related problems (DRPs), which significantly increased the length of stay from 4.4 (SD = 3.3) to 5.4 (SD = 3.6) days (p = 0.0001). DRPs were defined according to the Pharmaceutical Care Network Europe (PCNE) classification system as any event or circumstance involving pharmacotherapy that interferes or may interfere with desired health outcomes. In this study, DRPs were categorized into three main domains: indication problems (e.g., lack of prescription despite a clear indication), effectiveness problems (e.g., the treatment does not control adequately blood pressure), and safety problems (e.g., adverse drug reactions or inappropriate dosages). Patients exhibiting DRPs related to effectiveness showed a significantly increased risk of prolonged hospitalization, with an odds ratio of 3.73 (95% CI: 1.87–7.46). Similarly, those with DRPs related to blood pressure control—a subset of safety problems—had an odds ratio of 2.73 (95% CI: 1.43–5.19). These findings highlight the critical need for effective pharmaceutical care to minimize DRPs and their impact on postpartum recovery.
Altered biochemical parameters
In the study by Moroy et al. (2007) [16], risk factors related to changes in biochemical parameters were examined. The 98 patients were divided into two groups: short-term hospital stay (n = 33, 1–3 days) and long-term hospital stay (n = 65, four days or more). Among the patients analyzed, 3.03% of the short-term group (hospitalization ≤ 3 days) and 15.38% of the long-term group (hospitalization > 3 days) had a history of treatment with antihypertensive drugs before delivery (p = 0.049). Specific laboratory abnormalities, including elevated fibrinogen (p = 0.048), urea (p = 0.05), alanine transaminase (ALT) (p = 0.035), and aspartate transaminase (AST) (p = 0.040), were significantly correlated with hospital stays exceeding 3 days. Furthermore, the long-term hospitalization group exhibited diastolic blood pressure levels above 10 mmHg (p = 0.006). These findings suggest that these factors may not only indicate a prolonged length of stay but also reflect the underlying severity of the disease, as biochemical and hematological alterations are characteristic of more severe cases of preeclampsia.
Severity of preeclampsia
In the study by Xue et al. (2023)18, the severity of preeclampsia was also considered a factor affecting the length of hospital stay for pregnant women. The researchers found that women with severe or early-onset preeclampsia tended to have a longer hospital stay (5.7 days) and a greater risk of developing recurrent postpartum hypertension, severe preeclampsia (odds ratio 4,111, 95% CI: 1,236 a 13,271, p = 0,016), and early-onset preeclampsia (odds ratio 3,539, 95% CI: 1,049 an 11,472, p = 0,034) than women with mild or late-onset preeclampsia (4.5 days).
In study by Li and colleagues (2022) the severity of preeclampsia played a role in the length of hospital stay. Women with severe or early-onset preeclampsia had prolonged hospital stays of 5.4 to 5.6 days, which were significantly longer than those with mild (4.1 days) or late-onset preeclampsia (4.4 days) (p = 0.0001 or p < 0.0001, respectively).
Intrauterine Growth Restriction (IUGR)
In a study by Li and colleagues (2022) [20], intrauterine growth restriction (IUGR) emerged as a significant factor contributing to prolonged hospital stays for pregnant women with preeclampsia. Women with preeclampsia complicated by IUGR had a significantly longer duration of hospitalization (5.3 days) than those without IUGR (4.3 days) (95% CI: p = 0.0001, -0.98 [-1.48, -0.49]). Increased severity of placental dysfunction in IUGR cases requires closer maternal monitoring and management. Additionally, neonates with IUGR often require specialized care, such as admission to a Neonatal Intensive Care Unit, contributing to prolonged maternal hospitalization. These factors underscore the greater clinical complexity of preeclampsia with IUGR and the need for extended observation [20].
The type of delivery also influenced hospital stay duration, with 34 women with preeclampsia having a vaginal birth (average days: 3.4) and 174 women with preeclampsia undergoing cesarean section (average days: 5.8). Furthermore, the severity of preeclampsia played a role in the length of hospital stay. Women with severe or early-onset preeclampsia had prolonged hospital stays of 5.4 to 5.6 days, which were significantly longer than those with mild (4.1 days) or late-onset preeclampsia (4.4 days) (p = 0.0001 or p < 0.0001, respectively).
Congestive Heart Failure (CHF)
The study by Elkattawy et al. (2024) investigated the impact of CHF on women with preeclampsia and found CHF to be a significant factor associated with prolonged hospital stays. Patients with CHF had a longer mean length of stay (6 days vs. 4 days, p < 0.001) and were at increased risk for severe complications such as cardiac arrest (a OR 4.635, p = 0.004), ventricular tachycardia (a OR 17.487, p < 0.001), and pulmonary embolism (a OR 6.987, p < 0.001) [21].
Ventricular tachycardia
The study by Elkattawy et al. (2024) identified ventricular tachycardia as a rare but significant complication in preeclamptic patients, occurring in 0.04% of cases. Patients with ventricular tachycardia had a substantially prolonged hospital stay (7.16 days vs. 4.13 days, p = 0.001) and were more likely to experience severe outcomes, including cardiac arrest, postpartum hemorrhage, and the need for invasive procedures such as pacemaker implantation and heart catheterization. Predictors of ventricular tachycardia included pre-existing conditions such as congestive heart failure, atrial fibrillation, and obstructive sleep apnea [22].
Assessment of methodological quality
The studies included in this review were primarily cohort and case–control studies, with an average score of eight stars, indicating good methodological quality. However, there was notable heterogeneity among the studies, including variations in design and sample size. This heterogeneity may decrease the comparability of results both within and between studies, which should be taken into account when interpreting the findings. Further details of the study quality assessment are provided in Table 2.
Strengths and limitations
This study has both strengths and limitations. Notably, this inaugural review delved into the risk factors influencing extended postpartum stays among these patients, and meticulous efforts were undertaken to mitigate data heterogeneity. The inclusion of case‒control and cohort studies, which are known for their robustness in identifying risk factors, adds strength to the analysis. Furthermore, the study quality assessment utilized a widely recognized tool tailored for this purpose. The review’s inclusion of articles published not only in English but also in Portuguese or Spanish broadens its scope, and comprehensive searches across major scientific health literature databases were conducted.
It is important to note that the conditions and severity levels varied across the included studies, which may influence the comparability of findings. While some studies focused on severe preeclampsia cases requiring intensive monitoring, others included patients with milder forms of the condition. This heterogeneity in patient profiles and clinical settings highlights the need for caution when interpreting aggregated results, as variations in baseline health status, treatment protocols, and resource availability may impact the observed outcomes.
link







