ICBs told to give GPs extra training on postnatal checks

NHS England has asked ICBs to implement ‘additional training’ for GPs on postnatal consultations, focusing on physical recovery and mental health.
Local commissioners must strengthen the uptake of postnatal checks, by ensuring all eligible women receive a formal invitation, NHSE has said in new guidance.
And GP practices should be encouraged to prioritise women ‘at higher risk of poorer outcomes’, ensuring these women attend the checks and ‘engage with the review process’.
The new guidance is meant to support ICBs to ‘improve the postnatal care experience’ and both short and long-term maternal and infant health, recommending actions for ICBs and providers to ‘consider taking’.
NHS England said that ICBs should ensure women and babies receive ‘safe, personalised and joined-up care’, including a choice of ‘accessible support’ outside hospital environments and ‘smooth transitions’ to health visiting and GP services.
Commissioners should ensure all professionals providing postnatal care receive training in areas including:
- contraception choices and safe pregnancy spacing
- infant feeding (including breastfeeding support)
- trauma-informed care and identifying where mental health support may be needed
- bereavement care
However, GPs specifically should receive extra training. The recommendations added: ‘[ICBs should] implement additional training for GPs to support high-quality maternal 6-8-week postnatal consultations, focusing on physical recovery and mental health.’
Measures should also be implemented to make sure that GPs are informed in cases of perinatal loss or neonatal admission, to ensure ‘compassionate and tailored support’.
The RCGP said that they are ready to work with NHS England and partners to improve postnatal care, but that guidance ‘must be matched with the capacity to deliver it in practice’.
The GP-relevant recommendations in full
Deliver targeted training and development for professionals
- Ensure all professionals providing postnatal care receive training in areas such as:
- contraception choices and safe pregnancy spacing
- pelvic health and management of long-term conditions
- infant feeding (including breastfeeding support)
- trauma-informed care and identifying where mental health support may be needed
- bereavement care, including understanding local pathways and providing sensitive, compassionate care
- social determinants of health, ensuring professionals apply a making every contact count (MECC) approach to promote healthy behaviours, signposting and addressing wider factors affecting postnatal health
- Implement additional training for GPs to support high-quality maternal 6–8-week postnatal consultations, focusing on physical recovery and mental health. Refer to GP six to eight week maternal postnatal consultation: what good looks like.
Strengthen the uptake and experience of the 6–8-week postnatal GP consultation
- Increase the uptake and quality of the GP maternal postnatal consultation by ensuring all eligible women receive a formal invitation and actively encouraging its uptake.
- Implement measures to ensure GPs are informed in cases of perinatal loss or neonatal admission, to ensure compassionate and tailored support before, during and after the consultation.
- Encourage GP practices to prioritise women at higher risk of poorer outcomes, ensuring these women attend and engage with the review process. This should be achieved through proactive, personalised support and a proportionate universalism approach, tailoring and targeting care to meet specific needs while maintaining equitable access for all women.
Source: NHS England
In guidance updated last year, NHS England clarified that all GPs should be trained to undertake this consultation in GP specialty training and ‘should seek to update their knowledge and skills on a regular basis’.
The consultation is ‘universal’, it should be offered to all women, including those whose baby has died or does not reside with them for any reason (e.g. surrogacy, local authority care) and was included in the GP contract in 2020/21.
As well as reviewing maternity discharge letters, GPs should also use the consultation to review any pre-existing conditions where management may have been paused or altered or conditions that arose in pregnancy such as gestational diabetes.
Mental health should be a priority in the consultation, ahead of recovery or other conditions and every woman should be asked about it every time she is seen.
Identifying and addressing severe mental illness such as severe depression and postpartum psychosis should take precedent over other areas that can be addressed at another time.
RCGP chair Professor Victoria Tzortziou Brown said that additional training ‘may be helpful’ for some clinicians, but it cannot replace the need for ‘protected time, staffing and continuity’.
She added that improving postnatal care depends on ‘genuine integration’ between maternity services, health visitors and general practice, with ‘timely information sharing and appropriate resourcing’.
She said: ‘We know many women feel their postnatal concerns are not always fully heard or addressed, and improving their experience must be at the heart of efforts to strengthen postnatal care.
‘GPs are already highly trained to manage the complex physical and mental health needs that can arise during and after pregnancy. Where postnatal care does not meet expectations, this should not be assumed to reflect a lack of GP skills or knowledge.
‘More often, the barriers are lack of time, workforce pressures, poor continuity of care and fragmented information from maternity services.
‘High-quality postnatal care relies on having the time to listen and address multiple concerns, but this is increasingly difficult in a system focused on rapid access rather than meaningful, continuous care.’
Professor Azeem Majeed, head of the department of primary care and public health at Imperial College London, told Pulse that the new guidance ‘reinforces the central role of GPs’ in delivering personalised postnatal care, but that sustainable implementation will ‘depend on adequate support for primary care’.
He said: ‘The guidance highlights the need for far better coordination between maternity services, health visitors and primary care, including timely, comprehensive discharge information and clearer pathways for women with ongoing risks or complications.
‘For general practices, this will require active engagement in local ICB-led pathway development. The toolkit also places tackling inequalities at the heart of postnatal care.
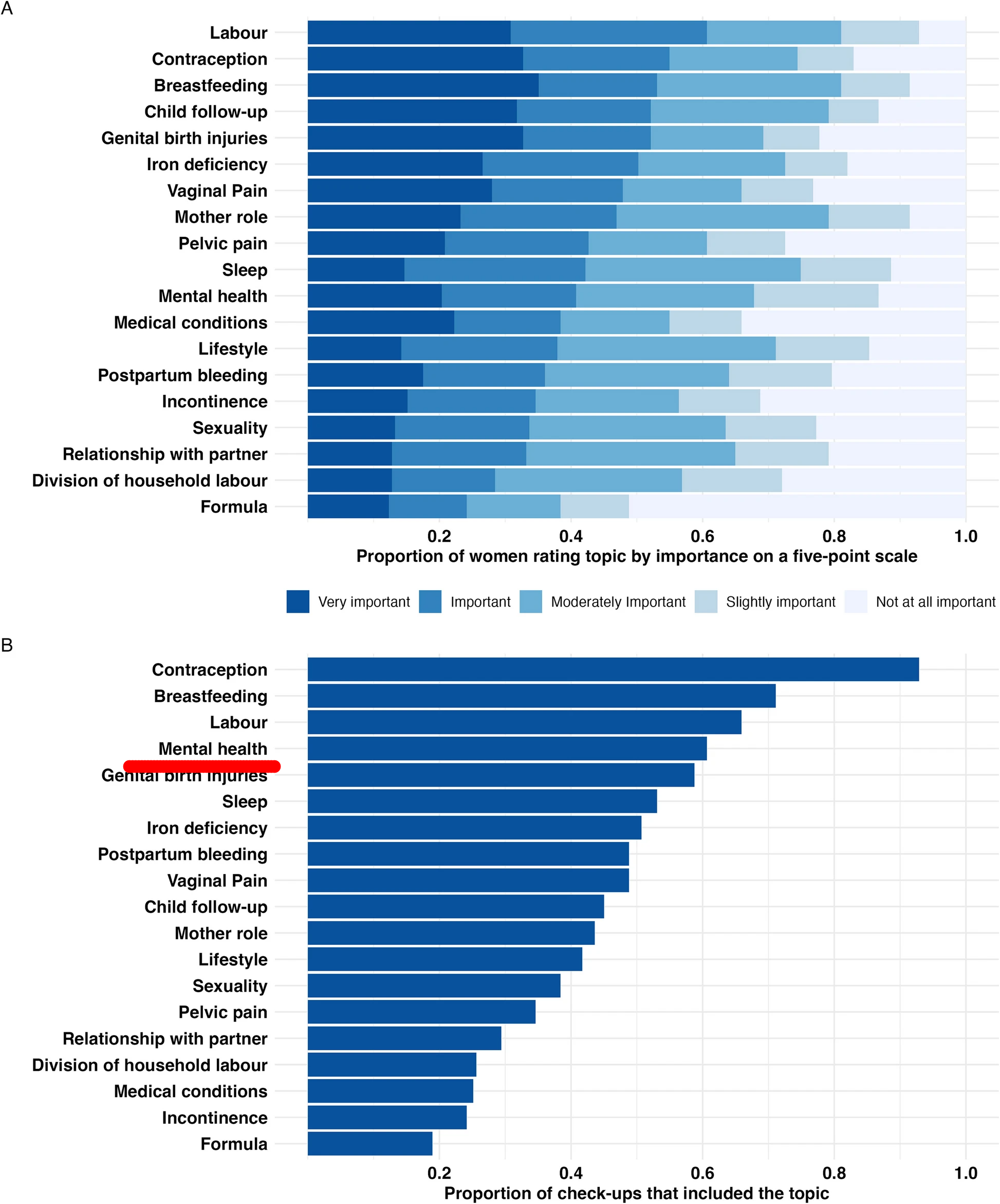
‘Practices will need to adopt proactive approaches to reach women at higher risk of poor outcomes, improve uptake of postnatal checks, and embed key public health interventions such as contraception, smoking cessation and infant feeding support.
‘Finally, the guidance calls for investment in workforce development, recognising that GPs and practice teams need the training, time and resources to deliver consistently excellent postnatal care.’
link